In nursing education, flexibility is no longer a differentiator—it’s the expectation.
Online, hybrid, evening, weekend, accelerated—you name it, students can find a version of it. Across the country, colleges are racing to launch new tracks and expand capacity. RN-to-BSN programs are booming. Online options are multiplying. Clinical partnerships are being stretched thin.
The pressure to adapt and scale is real. But in the midst of this expansion, one thing still separates great programs from the rest: quality.
Not marketing gloss. Not modality. But consistent, clinical-grade, accreditation-aligned quality—in every course, at every level, for every student.
The programs that figure out how to balance access with rigor? They’ll be the ones that stand out and that last.
The Demand Is Real—and It’s Not Slowing Down
We don’t need more speculation—we need more nurses. According to the U.S. Bureau of Labor Statistics, the U.S. healthcare system will need more than 200,000 new registered nurses each year through 2031 just to keep pace with retirements and new care demands BLS.
That pressure is already reshaping nursing education.
Across the country, nursing schools are expanding to meet surging demand. According to the American Association of Colleges of Nursing, enrollment in entry-level baccalaureate nursing programs grew by 5.6% in 2022, marking two decades of consistent growth in undergraduate nursing education. Simultaneously, RN-to-BSN programs enrolled more than 77,000 students that same year, reflecting increased interest from working nurses seeking flexible, advanced credentials. These trends have pushed many colleges to increase cohort sizes, offer alternative formats, and fast-track faculty hiring—all while trying to maintain rigorous academic and clinical standards.
Accelerated second-degree programs, online RN-to-BSN pathways, and flexible entry routes are bringing more diverse learners into nursing than ever before. And institutions are building new delivery models to meet that demand. In fact, nearly 40% of deans surveyed in 2024 said they plan to increase the number of online lab courses offered online.
But here’s the hard part: faster doesn’t mean better—unless you’re intentional about quality.
Flexibility Isn’t Optional Anymore
The modern nursing student isn’t a 20-year-old living on campus.
They’re older. More likely to have jobs and families. Many are returning to school after time in the workforce, seeking career pivots or advancement opportunities. According to the National League for Nursing, nearly a third of nursing students are over age 30.
For this audience, flexibility isn’t a “nice to have”—it’s the only reason school is even on the table.
That’s why online and hybrid models are growing. Asynchronous lectures, stackable credentials, and weekend intensives are opening doors. And these flexible options are vital for access and equity. But they don’t guarantee readiness.
Flexibility Draws Students In But Quality Keeps Them Enrolled
There’s a growing clinical confidence gap among online and accelerated learners—and most faculty know exactly where it comes from.
You can stream a lecture. You can simulate a scenario. But you can’t learn to take a blood pressure—or manage an injection—through a slideshow.
The reality is this: students need real practice with real tools. Especially in foundational courses like Nursing Fundamentals, Anatomy & Physiology, and Microbiology.
That’s where the first cracks tend to show in new program models. Many institutions move quickly to offer hybrid or accelerated courses—but forget to ask:
Which parts of this course actually require touch?
Where do we risk losing rigor?
These aren’t just academic questions. Students who start behind in lab-based foundational courses often never recover. According to a study out of National American University, community college nursing students who received a B or C in foundational A&P courses were significantly less likely to complete their programs on time.
Without strong, hands-on training early, students carry knowledge gaps into med-surg, pharmacology, and clinical placements. And once they’re in the field, those gaps aren’t theoretical anymore.
That’s why the most competitive nursing programs take a strategic view. Programs that are successful design their models not just for enrollment growth, but for clinical outcomes. They ask:
- How do we give students flexibility—without sacrificing fidelity?
- What skills are being built, and where are they practiced?
- Are we preparing students for the NCLEX, or just passing them through modules?
🧠 Related read: Check out Upholding Quality Without Compromise to see how online nursing education can absolutely uphold rigorous standards—but only if it’s intentionally designed to preserve tactile learning.
Clinical Competency Is Still the Goal
Simulation has come a long way—and it’s a valuable part of modern nursing education. Virtual environments can support critical thinking, decision-making, and exposure to diverse clinical situations.
But simulations aren’t enough.
They don’t build muscle memory. They don’t replicate the feel of an actual blood pressure cuff. And they can’t fully prepare students for the unpredictable human element of care.
This isn’t just a philosophical stance—it’s a regulatory one. Accreditation bodies like CCNE and ACEN require programs to include in-person or tactile clinical training. Simulation can supplement, but it doesn’t replace. Students still need meaningful hands-on experience to demonstrate competence, safety, and sound judgment in clinical environments (ACEN Standards).
If your students are walking into clinicals unsure of how to hold a stethoscope or administer a subcutaneous injection, that’s not an online education problem—it’s a program quality problem.
Fundamentals Aren’t Optional
Every student has to start somewhere. And where they start matters.
Courses like Nursing Fundamentals aren’t just about checking boxes. They’re where students start building clinical instincts—how to manage infection control, work under time pressure, prioritize care, and build confidence in their own hands.
When Fundamentals is reduced to a packet or condensed into a simulation-only experience, no matter how highly sophisticated, students don’t get what they need. They don’t know how to troubleshoot tubing. They hesitate on wound care. They make preventable mistakes.
Early exposure to lab equipment, even in a hybrid or remote format, changes the trajectory. Students enter pharmacology or pathophysiology with more context. They retain key concepts better. They engage more deeply.
Institutional Strategies That Work
How can nursing programs strike the right balance between scale and rigor?
It starts with leadership—specifically, deans and department chairs willing to ask the hard questions and support faculty through the answers.
Train and support faculty. Transitioning to online or hybrid instruction is not just about uploading content. Instructors need support in labs, evaluating hands-on skills remotely, and maintaining consistency across sections and formats.
Invest where it counts. Whether through mailed lab kits, simulation labs, or clinical partnerships, institutions must commit real resources to clinical prep—not just digital infrastructure.
Audit and adapt. Monitor student outcomes, clinical feedback, and retention data. If certain cohorts are struggling in clinicals, trace the root. Is there a gap in the foundational experience? Are certain modalities shortchanging hands-on repetition?
The strongest programs aren’t necessarily the flashiest—they’re the ones with intentional design and internal accountability.
Compete on Quality, Not Just Convenience
The future of nursing education isn’t one-size-fits-all. But it does have one non-negotiable: students must graduate ready.
The institutions that will thrive in this new, crowded market aren’t the ones that scale the fastest. They’re the ones that scale wisely—preserving clinical rigor, supporting their faculty, and ensuring that flexibility doesn’t dilute standards. It’s the ones that ensure all students receive a meaningful and rigorous lab experience from wherever they take your course.
Excellence isn’t the tradeoff for access. It’s the outcome of getting it right. Pairing flexibility with clinical rigor will help you reach more students without lowering the bar. That’s how you stand out in a crowded field—and how you graduate nurses who are ready the moment they put on the scrubs.
Nursing students deserve that. So do the patients they will eventually care for.
Discover more articles
Research Reveals a Dual Prep Problem in STEM Courses & New Opportunities to Deliver Rigor at Scale
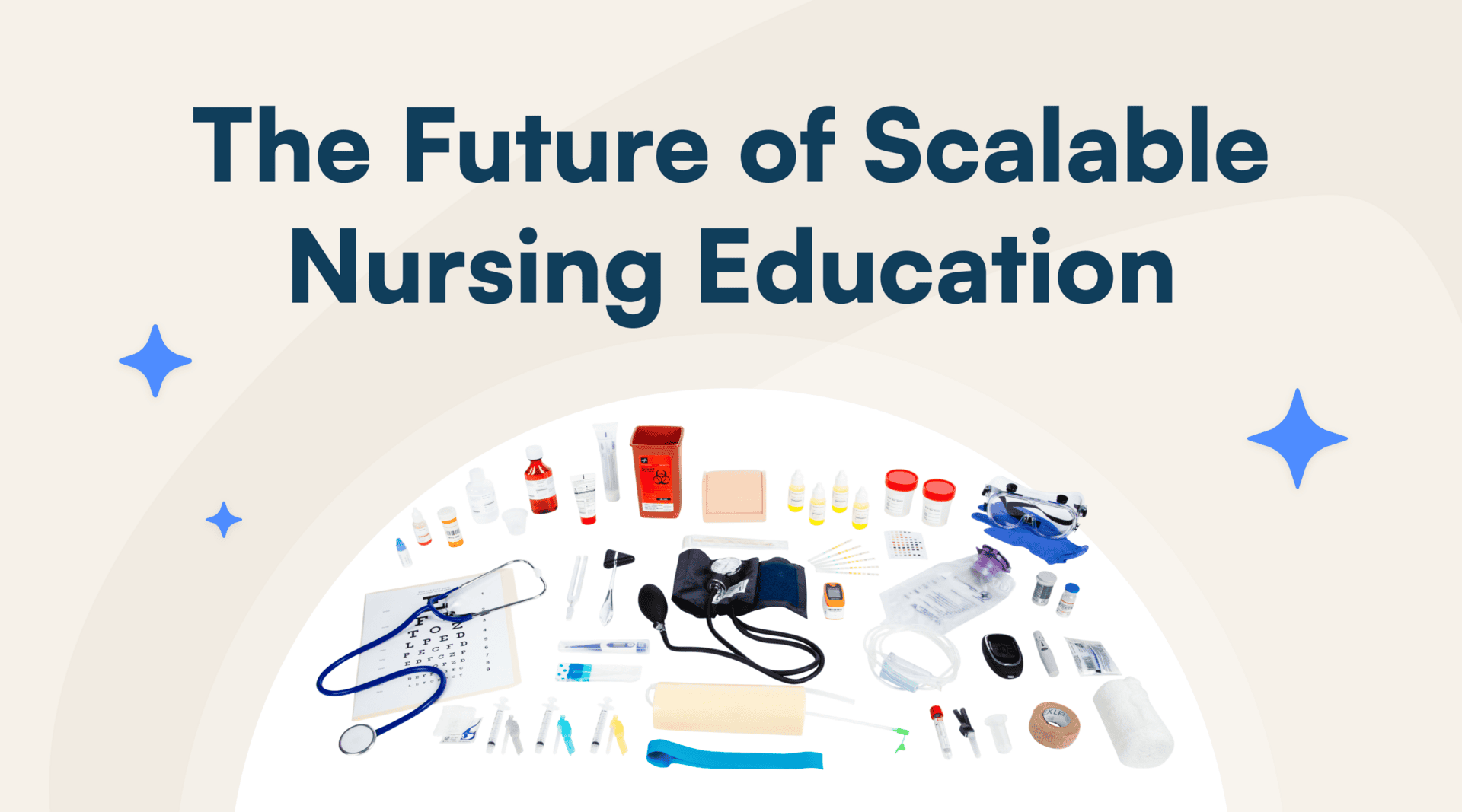
Science Interactive Launches New Nursing Fundamentals